Table of Contents
- Introduction
- Stem Cell Therapies
- Gene Editing Technologies
- Tissue Engineering
- Clinical Trials and Approvals
- Future Directions
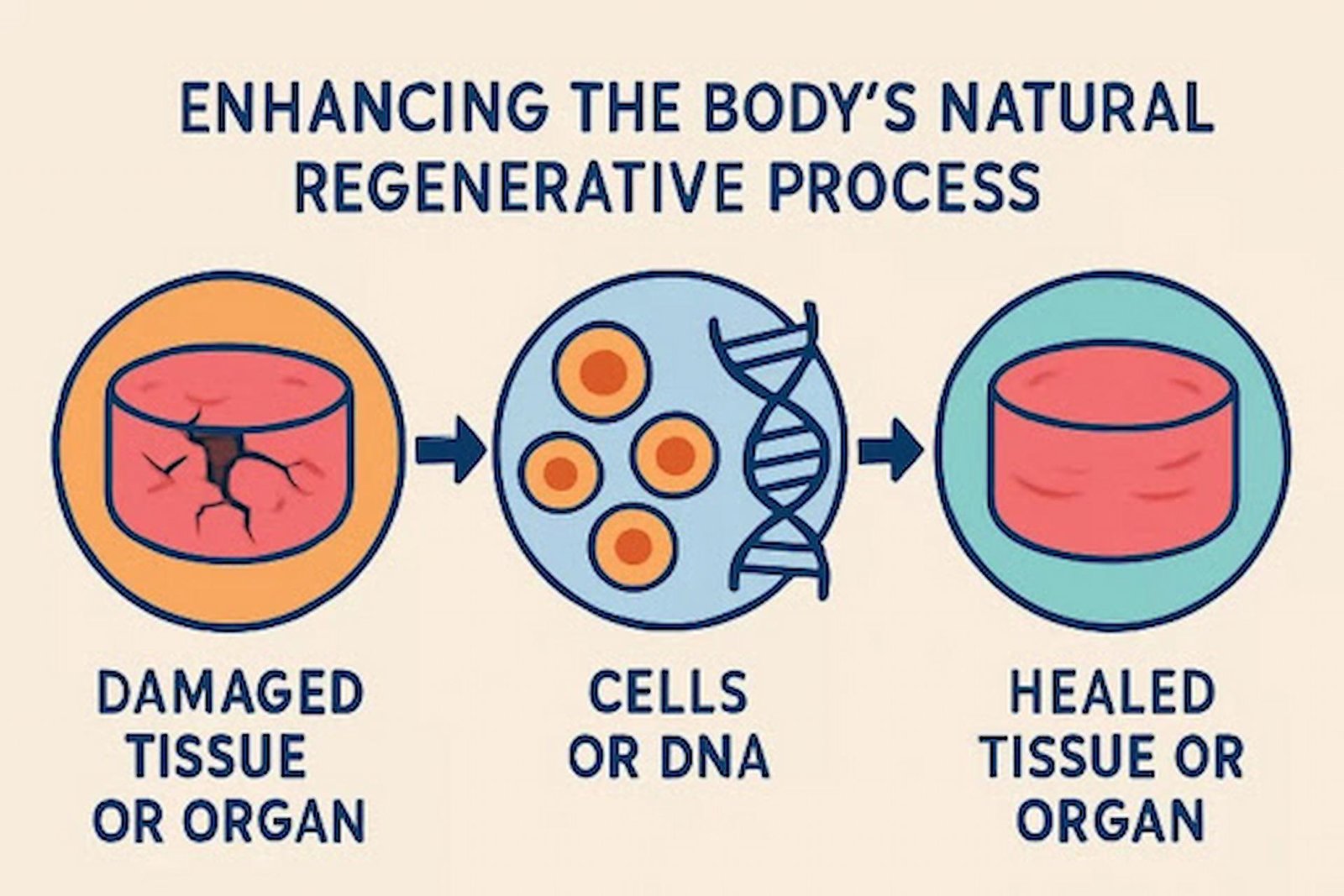
Regenerative medicine has emerged as a beacon of hope for millions suffering from chronic illnesses by leveraging the body’s intrinsic ability to heal, repair, and rejuvenate itself. Unlike traditional medical avenues that focus on alleviating symptoms, regenerative approaches strive to resolve the underlying issues causing disease. This difference marks a paradigm shift in the treatment of conditions once thought to be manageable at best, and never truly curable. With the introduction of procedures such as stem cell therapy, gene editing, and advanced tissue engineering, patients with ailments like diabetes, arthritis, neurodegenerative diseases, and autoimmune disorders are witnessing the dawn of new treatment possibilities. For people investigating a non-surgical solution for pain, regenerative medicine provides an attractive, minimally invasive option that can potentially address pain at its source. These medical advancements are redefining both patient outcomes and the broader potential for reversing chronic conditions instead of simply controlling them—heralding an era where true cellular healing is not only desired but increasingly achievable.
This field’s acceleration is fueled by technological innovation, supportive regulations, and a rapidly growing understanding of human biology at the cellular and genetic levels. As regenerative medicine expands its reach, it offers unprecedented opportunities for healthcare professionals to deliver more personalized, effective therapies. Patients stand to gain more than relief—they can look toward restoration of lost function and a return to active, fulfilling lives. The ripple effect of these breakthroughs is being felt across global healthcare, affecting not just treatment protocols but inspiring hope and empowerment for individuals who once faced limited options.
Stem Cell Therapies
Stem cell therapies stand at the forefront of revolutionary developments in regenerative medicine, offering the possibility to repair or replace damaged tissues and organs. Pluripotent stem cells, in particular, exhibit the unique ability to differentiate into any of the 200+ cell types found in the human body, creating immense therapeutic potential. For instance, recent advancements have enabled the transformation of these cells into insulin-producing beta cells, offering profound hope for people living with type 1 diabetes. According to recent clinical trials, lab-grown beta cell transplants have resulted in remarkable improvements in patients’ blood glucose management. Some trial participants were eventually able to forego insulin injections altogether, marking a milestone for diabetes care that addresses the disease at the cellular level rather than merely mitigating its symptoms.
The therapeutic scope of stem cell technology extends far beyond diabetes. Research teams across the globe are actively evaluating stem cell-based interventions for chronic heart failure, spinal cord injuries, osteoarthritis, and autoimmune diseases such as multiple sclerosis. Each of these conditions involves cells or tissues that have been irreversibly damaged by disease processes—and the regenerative capacity of stem cells unlocks new avenues for healing that were unimaginable just a decade ago. As methods and understanding improve, the safety profile, durability, and accessibility of these treatments are expected to rapidly increase, opening the door to long-term solutions for chronic health concerns that impair millions worldwide.
Gene Editing Technologies
Modern gene-editing tools, with CRISPR-Cas9 leading the way, are fundamentally reshaping what’s possible within regenerative medicine. These tools allow scientists and clinicians to precisely target and correct genetic mutations responsible for a wide range of hereditary conditions. In one landmark development in the treatment of sickle cell disease, for example, a patient’s own hematopoietic stem cells are harvested, the disease-causing gene is edited with CRISPR technology, and the corrected cells are reintroduced into the bloodstream. Initial results from these innovative procedures are nothing short of remarkable—patients are producing healthy red blood cells and, in some cases, are effectively cured of a life-threatening disorder that once dramatically shortened life expectancy and quality of life.
The potential applications of gene editing do not end with sickle cell disease. Researchers are actively pursuing similar genetic interventions for cystic fibrosis, certain inherited causes of blindness, muscular dystrophies, blood cancers, and more. These medical advances promise to not only halt disease progression but to fundamentally eradicate underlying causes. As gene editing becomes more refined and accessible, it paves the way for a future in which previously untreatable or fatal illnesses are rendered manageable—or even cured outright—through personalized genetic correction.
Tissue Engineering
Tissue engineering unites biological science with engineering principles to build living, functional tissues for patients in need of organ or tissue replacement. This field is rapidly making headway, with achievements such as bioengineered liver organoids garnering global attention. These miniaturized, three-dimensional organs stand in for their human counterparts in drug testing and, potentially, transplantation. For those with liver disease, engineered organoids could one day offer life-saving alternatives that bypass critical obstacles like donor shortages and immune rejection. The successful cultivation of organs in the laboratory also supports a new frontier in understanding disease mechanisms in a controlled environment—essential for accelerating drug development and minimizing patient risk.
Beyond organoids, tissue engineering already supports vital clinical applications. Synthetic skin grafts derived from cultured patient cells accelerate wound healing for burn victims. Biodegradable scaffolds facilitate the regeneration of new cartilage for those with arthritic joint degeneration, and new blood vessels are being constructed and implanted for cardiovascular repairs. As these approaches mature, the customization and availability of engineered tissues are set to expand further, offering more individuals personalized options for restoring normal function following disease or trauma.
Clinical Trials and Approvals
Moving regenerative therapies from the research lab to the clinic is a critical, highly regulated process. Recent progress includes landmark regulatory approvals that underscore the growing trust in cellular and genetic therapies. One striking example is the U.S. Food and Drug Administration’s approval of mesenchymal stromal cell therapy aimed at pediatric patients suffering from steroid-refractory acute graft-versus-host disease—a serious, life-threatening complication following bone marrow transplantation. This approval is more than a clinical milestone; it signifies mounting confidence in the safety and effectiveness of cell-based regenerative therapies and signals their move from experimental to mainstream medicine.
In parallel, hundreds of additional clinical trials are exploring regenerative treatments for chronic pain, heart disease, diabetes, autoimmune and neurodegenerative disorders. This robust research pipeline reflects the field’s momentum, with promising therapies in late-stage development that could soon yield new tools for clinicians and new hope for patients. The pace of regulatory review and approval is expected to continue accelerating as experience grows and evidence mounts, further integrating regenerative medicine into standard healthcare.
Future Directions
The horizon for regenerative medicine is bright, brimming with efforts to refine treatment safety, efficacy, and accessibility. Scientists continue to pursue less invasive delivery systems and ever-greater precision for gene editing platforms, aiming to minimize unintended effects and boost clinical success. One promising frontier is research on exosomes—tiny, cell-released vesicles found to carry vital biological messages that promote healing and reduce inflammation. Exosomes are under investigation as a cell-free regenerative therapy that could deliver healing effects without the risks and logistical complexities of traditional stem cell transplantation, opening new avenues for safer, more scalable interventions.
Breakthroughs are increasingly driven by cross-disciplinary collaboration among biologists, engineers, materials scientists, and digital technology experts. By pooling expertise, researchers can accelerate the integration of artificial intelligence, nanotechnology, and biomaterials into regenerative medicine, ushering in smarter, faster, and more personalized therapy development. As these next-generation therapies enter the clinic, regenerative medicine will continue to shift the healthcare paradigm—offering cures and proper restoration to conditions once managed only with long-term medication or surgery. Regenerative medicine stands on the brink of transforming the healthcare landscape for those with chronic illnesses, renewing hope for patients everywhere who are seeking comprehensive and sustainable healing through science and innovation.